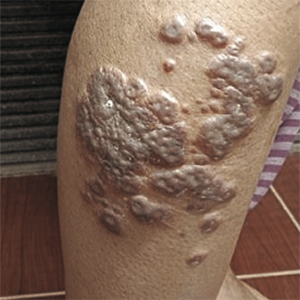
Cutaneous anthrax in patient with type 2 diabetes mellitus
HTML: 21
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Anthrax is a zoonotic disease caused by Bacillus anthracis, which is transmitted to humans from infected animals. Transmission occurs when there is a contact with animals or products from animals infected with anthrax. Anthrax infection is an important public health problem in developing countries. Indonesia is one of the countries where zoonotic anthrax forms can still be found. The most common entrance route for anthrax spores is the skin. Although skin anthrax usually resolves on its own, complications can arise in untreated cases. Underlying systemic disorders such as diabetes mellitus can disrupt the clinical picture and cause atypical presentation. A 50-year-old woman who works as a farmer with a history of diabetes mellitus, is treated at a local hospital with complaints of fever and inflamed lesions in the lower right leg. An anthrax outbreak has been reported in the area where she lives. At clinical examination regional swelling was found and the appearance of blackish lesions accompanied by pus around the wound. Laboratory tests documented by ELISA an increased titer of anthrax antibodies. The patient was given antibiotic therapy with a combination of penicillin G and ciprofloxacin intravenously and experienced healing from skin lesions. We can conclude that comorbid diseases such as diabetes mellitus can obscure clinical manifestations of skin anthrax and causes systemic symptoms. With appropriate management, skin anthrax lesions in patients with comorbid diabetes mellitus can heal with good results.
Oncu S, Oncu S, Sakarya S. Anthrax – an overview. Medical Sci Monit 2003;9:RA276-83.
Wenner KA, Kenner JR. Anthrax. Derm Clin 2004;22:247-56. DOI: https://doi.org/10.1016/j.det.2004.03.001
Thappa DM, Karthikeyan K. Anthrax: an overview within the Indian subcontinent. Int J Dermatol 2001;40:216-22. DOI: https://doi.org/10.1046/j.1365-4362.2001.01174.x
Doganay M. Anthrax. In: Cohen, J, Powderly, WG, eds. Infectious Diseases. Mosby, London, 2nd edn, 2004. pp 1685-9.
Bell DM, Kozarsky PE, Stephens DS. Clinical issues in the prophylaxis, diagnosis, and treatment of anthrax. Emerg Infect Dis 2002;8:222-5. DOI: https://doi.org/10.3201/eid0802.01-0521
Chensue SW. Exposing a killer: pathologists angle for anthrax. Am J Pathol 2003;163:1699-702. DOI: https://doi.org/10.1016/S0002-9440(10)63526-2
Dixon TC, Meselson M, Guillemin J, Hana PC. Anthrax. N Engl J Med 1999;341:815-26. DOI: https://doi.org/10.1056/NEJM199909093411107
Carucci JA, McGovern TW, Norton SA et al. Cutaneous anthrax management algorithm. J Am Acad Dermatol 2002;47:766-9. DOI: https://doi.org/10.1067/mjd.2002.128381
Dib EG, Dib SA, Korkmaz DA, et al. Nonhemolytic, non-motile Gram-positive rods indicative of Bacillus anthracis. Emerg Infect Dis 2003;9:1013-5. DOI: https://doi.org/10.3201/eid0908.030205
Demirdag K, Ozden M, Saral Y et al. Cutaneous anthrax in adults: a review of 25 cases in the eastern Anatolian region of Turkey. Infection 2003;31:327-30. DOI: https://doi.org/10.1007/s15010-003-3169-3
Copyright (c) 2022 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.





 https://doi.org/10.4081/dr.2022.9426
https://doi.org/10.4081/dr.2022.9426



