Atopic dermatitis: a brief review of recent advances in its management
Accepted: 23 February 2023
HTML: 29
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
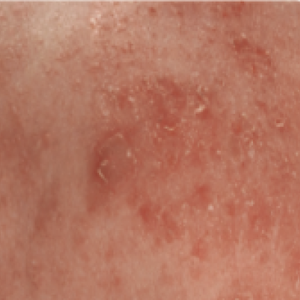
Atopic dermatitis (AD) is a common inflammatory skin disorder characterized by recurrent eczematous lesions and intense itching. The disorder affects people of all ages and ethnicities, has a substantial psychosocial impact on patients and relatives, and is the leading cause of the global burden of skin diseases. Atopic dermatitis is associated with an increased risk of multiple comorbidities, including food allergies, asthma, allergic rhinitis, and mental health disorders. The pathophysiology is complex and involves a strong genetic predisposition, epidermal dysfunction, and T-cell-driven inflammation. Although type-2 mechanisms are dominant, there is increasing evidence that the disorder involves multiple immune pathways. Until recently, the management of AD rested mainly on the judicious use of emollients, topical steroids, and topical calcineurin inhibitors in the majority of patients, and systemic immunosuppressants were advocated in severely diseased patients. However, in the last few years, new therapeutic strategies have been designed and developed to target the various steps in the chain of molecular events that lead to the AD phenotype. This review highlights the recent advancements in the management of AD.
Thomsen SF. Atopic dermatitis: natural history, diagnosis, and treatment. ISRN Allergy 2014;2014:354250.
Silverberg, JI, Barbarot S, Gadkari A, et al. Atopic dermatitis in the pediatric population: a cross-sectional, international epidemiologic study. Ann. Allergy Asthma Immunol 2021;126:417-28.e2.
Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol 1994;30:35-9.
Eichenfeld LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol 2014;70:338-51.
Spergel JM, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol 2003;112:S118-27.
Tsakok T, Marrs T, Mohsin M, et al. Does atopic dermatitis cause food allergy? A systematic review. J Allergy Clin Immunol 2016;137:1071-8.
Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol 2013;131:428-33.
Yang EJ, Sekhon S, Sanchez IM, et al. Recent developments in atopic dermatitis. Pediatrics 2018;142:e20181102.
Nakajima S, Nomura T, Common J, Kabashima K. Insights into atopic dermatitis gained from genetically defined mouse models. J Allergy Clin Immunol 2019;143:13-25.
Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab 2015;66:8-16.
Barbarot S, Auziere S, Gadkari A, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy 2018;73:1284-93.
Silverberg JI. Public health burden and epidemiology of atopic dermatitis. Dermatol Clin 2017;35:283-9.
Sandilands A, Terron-Kwiatkowski A, Hull PR, et al. Comprehensive analysis of the gene encoding filaggrin uncovers prevalent and rare mutations in ichthyosis vulgaris and atopic eczema. Nat Genet 2007;39:650-4.
Saini S, Pansare M. New insights and treatments in atopic dermatitis. Pediatr Clin North Am 2019;66:1021-33.
Weidinger S, Novak N. Atopic dermatitis. Lancet 2016;387:1109-22.
Mandlik DS, Mandlik SK. Atopic dermatitis: new insight into the etiology, pathogenesis, diagnosis and novel treatment strategies. Immunopharmacol Immunotoxicol 2021;43:105-25.
Gittler JK, Wang JF, Orlow SJ. Bathing and associated treatments in atopic dermatitis. Am J Clin Dermatol 2017;18:45-57.
Maliyar K, Sibbald C, Pope E, Sibbald RG. Diagnosis and management of atopic dermatitis: a review. Adv Skin Wound Care 2018;31:538-50.
Sher LG, Chang J, Patel IB, et al. Relieving the pruritus of atopic dermatitis: a meta-analysis. Acta Derm Venereol 2012;92:455-61.
Lucky AW, Leach AD, Laskarzewski P, Wenck H. Use of an emollient as a steroid-sparing agent in the treatment of mild to moderate atopic dermatitis in children. Pediatr Dermatol 1997;14:321-4.
Barnes L, Kaya G, Rollason V. Topical corticosteroid-induced skin atrophy: a comprehensive review. Drug Saf 2015;38:493-509.
Levin E, Gupta R, Butler D, et al. Topical steroid risk analysis: differentiating between physiologic and pathologic adrenal suppression. J Dermatolog Treat 2014;25:501-6.
Niedner R. Therapy with systemic glucocorticoids. Hautarzt 2001;52:1062-71. [Article in German].
Lübbe J, Friedlander SF, Cribier B, et al. Safety, efficacy, and dosage of 1% pimecrolimus cream for the treatment of atopic dermatitis in daily practice. Am J Clin Dermatol 2006;7:121-31.
Dotterud LK, Wilsgaard T, Vorland LH, Falk ES. The effect of UVB radiation on skin microbiota in patients with atopic dermatitis and healthy controls. Int J Circumpolar Health 2008;67:254-60.
Vähävihu K, Ylianttila L, Salmelin R, et al. Heliotherapy improves vitamin D balance and atopic dermatitis. Br J Dermatol 2008;158:1323-8.
Grabbe J, Welker P, Humke S, et al. High-dose ultraviolet A1 (UVA1), but not UVA/UVB therapy, decreases IgE binding cells in lesional skin of patients with atopic eczema. J Invest Dermatol 1996;107:419-22.
Huang JT, Abrams M, Tlougan B, et al. Treatment of Staphylococcus aureus colonization in atopic dermatitis decreases disease severity. Pediatrics 2009;123:808-14.
Kapur S, Watson W, Carr S. Atopic dermatitis. Allergy Asthma Clin Immunol 2018;14:52.
Roekevisch E, Spuls PI, Kuester D, et al. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol 2014;133:429-38.
Seger EW, Wechter T, Strowd L, Feldman SR. Relative efficacy of systemic treatments for atopic dermatitis. J Am Acad Dermatol 2019;80:411-6.e4.
Meggitt SJ, Gray JC, Reynolds NJ. Azathioprine dosed by thiopurine methyltransferase activity for moderate-to-severe atopic eczema: a double-blind, randomised controlled trial. Lancet 2006;367:839-46.
Simpson EL, Bruin-Weller M, Flohr C, et al. When does atopic dermatitis warrant systemic therapy? Recommendations from an expert panel of the International Eczema Council. J Am Acad Dermatol 2017;77:623-33.
Le Floc’h A, Allinne J, Nagashima K, et al. Dual blockade of IL-4 and IL-13 with dupilumab, an IL-4Rα antibody, is required to broadly inhibit Type 2 inflammation. Allergy 2020;75:1188-204.
Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med 2016;375:2335-48.
Beck LA, Thaçi D, Deleuran M, et al. Dupilumab provides favorable safety and sustained efficacy for up to 3 years in an open-label study of adults with moderate-to-severe atopic dermatitis. Am J Clin Dermatol 2020;21:567-77.
Eichenfield LF, Bieber T, Beck LA, et al. Infections in dupilumab clinical trials in atopic dermatitis: a comprehensive pooled analysis. Am J Clin Dermatol 2019;20:443-56.
Drucker AM, Ellis AG, Bohdanowicz M, et al. Systemic immunomodulatory treatments for patients with atopic dermatitis: a systematic review and network meta-analysis. JAMA Dermatol 2020;156:659-67.
Wollenberg A, Howell MD, Guttman-Yassky E, et al. Treatment of atopic dermatitis with tralokinumab, an anti-IL-13 mAb. J Allergy Clin Immunol 2019;143:135-41.
Paller AS, Siegfried EC, Thaçi D, et al. Efficacy and safety of dupilumab with concomitant topical corticosteroids in children 6 to 11 years old with severe atopic dermatitis: a randomized, double-blinded, placebo-controlled phase 3 trial. J Am Acad Dermatol 2020;83:1282-93.
Guttman-Yassky E, Blauvelt A, Eichenfield LF, et al. Efficacy and safety of lebrikizumab, a high-affinity interleukin 13 inhibitor, in adults with moderate to severe atopic dermatitis: a phase 2B randomized clinical trial. JAMA Dermatol 2020;156:411-20.
Deleanu D, Nedelea I. Biological therapies for atopic dermatitis: an update. Exp Ther Med 2018;17:1061-7.
Khattri S, Brunner P, Garcet S, et al. Efficacy and safety of ustekinumab treatment in adults with moderate-to-severe atopic dermatitis. Exp Dermatol 2017;26:28-35.
Chen YL, Gutowska-Owsiak D, Hardman CS, et al. Proof-of-concept clinical trial of etokimab shows a key role for IL-33 in atopic dermatitis pathogenesis. Sci Transl Med 2019;11:eaax2945.
Parnes JR, Sullivan JT, Chen L, Dias C. Pharmacokinetics, safety, and tolerability of tezepelumab (AMG 157) in healthy and atopic dermatitis adult subjects. Clin Pharmacol Ther 2019;106:441-9.
Holm JG, Thomsen SF. Omalizumab for atopic dermatitis: evidence for and against its use. G Ital Deramatol Venereol 2019;154:480-7.
Nezamololama N, Fieldhouse K, Metzger K, Gooderham M. Emerging systemic JAK inhibitors in the treatment of atopic dermatitis: a review of abrocitinib, baricitinib, and upadacitinib. Drugs Context 2020;9:2020-8-5.
Simpson EL, Sinclair R, Forman S, et al. Efficacy and safety of abrocitinib in adults and adolescents with moderate-to-severe atopic dermatitis (JADE MONO-1): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet 2020;396:255-66.
Ferreira S, Guttman-Yassky E, Torres T. Selective JAK1 inhibitors for the treatment of atopic dermatitis: focus on upadacitinib and abrocitinib. Am J Clin Dermatol 2020;21:783-98.
Pavel AB, Song T, Kim HJ, et al. Oral janus kinase/SYK inhibition (ASN002) suppresses inflammation and improves epidermal barrier markers in patients with atopic dermatitis. J Allergy Clin Immunol 2019;144:1011-24.
Wood H, Chandler A, Nezamololama N, et al. Safety of janus kinase (JAK) inhibitors in the short-term treatment of atopic dermatitis. Int J Dermatol 2022;61:746-54.
Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol 2016;75:494-503.e6.
Pao-Ling Lin C, Gordon S, Her MJ, Rosmarin D. A retrospective study: application site pain with the use of crisaborole, a topical phosphodiesterase 4 inhibitor. J Am Acad Dermatol 2019;80:1451-3.
Simpson EL, Imafuku S, Poulin Y, et al. A phase 2 randomized trial of apremilast in patients with atopic dermatitis. J Invest Dermatol 2019;139:1063-72.
Peppers J, Paller AS, Maeda-Chubachi T, et al. A phase 2, randomized dose-finding study of tapinarof (GSK2894512 cream) for the treatment of atopic dermatitis. J Am Acad Dermatol 2019;80:89-98.e3.
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.





 https://doi.org/10.4081/dr.2023.9678
https://doi.org/10.4081/dr.2023.9678



